Indications for anticoagulant and antiplatelet combined therapy
BMJ 2017; 359 doi: https://doi.org/10.1136/bmj.j3782 (Published 05 October 2017) Cite this as: BMJ 2017;359:j3782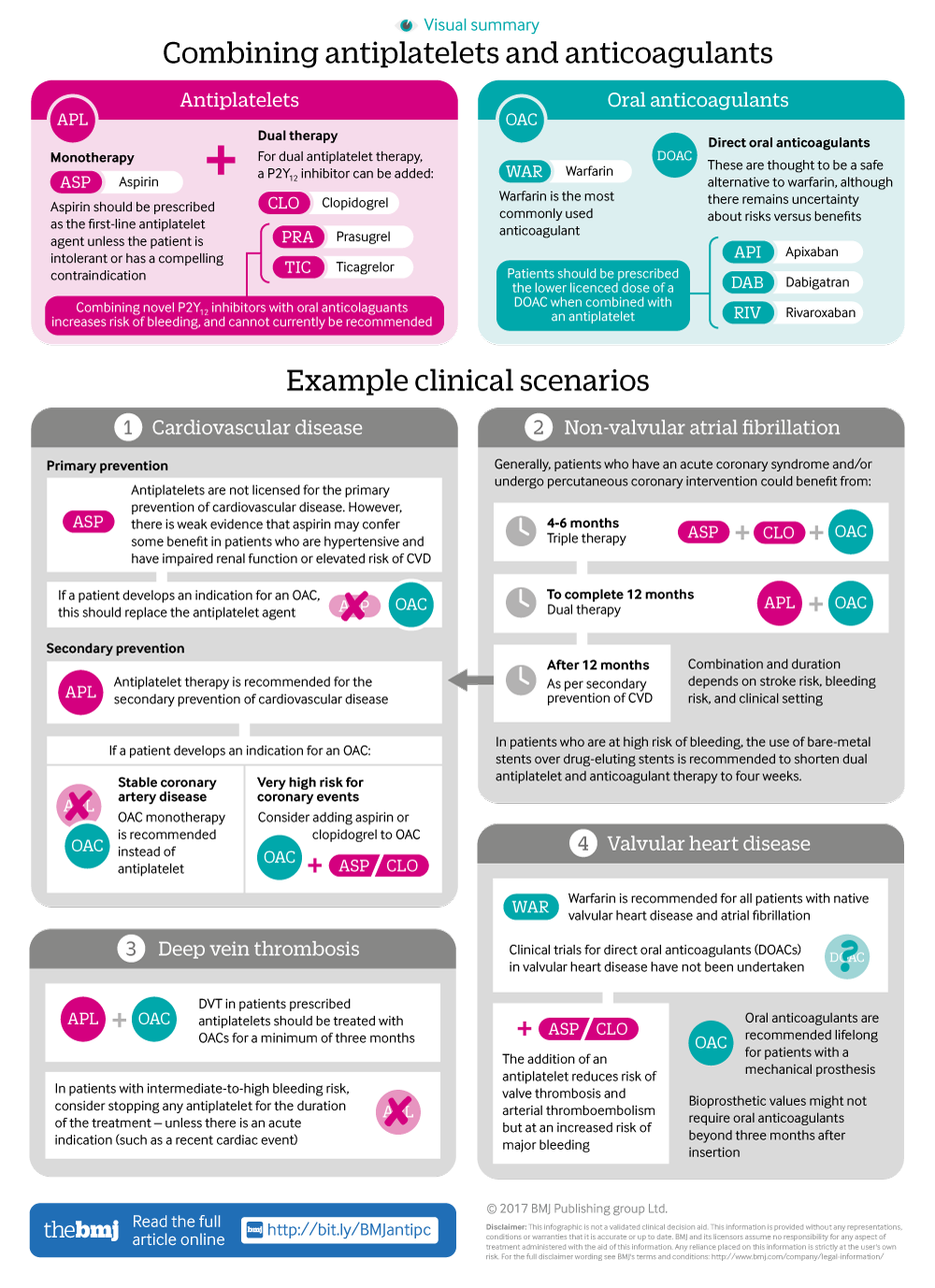
Infographic available
A visual summary of approaches for combining anticoagulants and antiplatelets, along with clinical scenario examples
- Christopher N Floyd, clinical lecturer in clinical pharmacology and therapeutics,
- Albert Ferro, professor of clinical pharmacology
- Department of clinical pharmacology, cardiovascular division, British Heart Foundation Centre of Research Excellence, King’s College London, London, UK
- Correspondence to A Ferro albert.ferro{at}kcl.ac.uk
- Accepted 17 July 2017
What you need to know
Combination antithrombotic treatment increases the risk of bleeding, and this risk should be estimated and discussed with patients to guide treatment decisions (eg, using risk scores such as HAS-BLED)
In most patients with independent indications for both antiplatelet and oral anticoagulant therapy the pathophysiology will intersect and combination antithrombotic treatment may not be necessary
When co-prescribing, check that the patient is not prescribed medication that will increase bleeding risk further (eg, non-steroidal anti-inflammatory drugs) and consider the addition of an H2 antagonist or proton pump inhibitor.
Antithrombotic medications reduce thromboembolic events by inhibiting platelet aggregation and coagulation. Antiplatelet drugs and oral anticoagulants are examples of antithrombotic medications and are among the most commonly prescribed drugs in both primary and secondary care.1 Clinicians are familiar with their use, however antiplatelets and oral anticoagulants are the drug classes most commonly implicated in adverse drug reactions occurring both in the community and in hospital.23 Increasing numbers of patients have an indication for combination antiplatelet and oral anticoagulant therapy. For example, more than one million people in the UK have atrial fibrillation, of whom approximately one third also have an indication for antiplatelet therapy as secondary prevention.4 Despite the need to understand the balance between benefit and risk, there are limited randomised data investigating antithrombotic co-prescription. Current guidelines are therefore based on expert opinion and the extrapolation of non-randomised data.
Who might need co-prescription?
Patients can develop independent indications for antiplatelet and oral anticoagulant therapy, but in most cases the pathophysiology will intersect. The relationship between cardiovascular disease and atrial fibrillation is the typical example, where one fifth of patients presenting with atrial fibrillation will subsequently require coronary intervention, and up to one fifth of acute coronary syndrome (including ST elevation myocardial infarction, non-ST elevation myocardial infarction, and unstable angina) presentations develop atrial …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £173 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£38 / $45 / €42 (excludes VAT)
You can download a PDF version for your personal record.
